Last month, the Centers for Medicare and Medicaid Services its released its Star Ratings findings for 2020 with some great news: More plans rated four stars or higher this year compared to the year before.
To get more specific, more than 50 percent of plans rated four and above, up from 45 percent. In addition, the enrollment weighted average increased from 4.06 last year to 4.16 this year. Twenty plans earned five stars, yet another sign of continued improvements.
Why Does it Matter?
Most Medicare Part D and Medicare Advantage plans understand the importance of Star Ratings. The ratings are put out annually by the Centers for Medicare and Medicaid Services to give beneficiaries a look at the quality of the health plan before they sign up. Star Ratings focus on aspects of high-quality care within the control of the plan. They provide a complete, accurate, reliable, and valid picture of a program. Star Ratings also are used for compliance and monitoring, and measure aspects of a plan that are relevant and important to beneficiaries. CMS looks to NCQA, PQA and others for measure concept development, endorsement, and specifications.
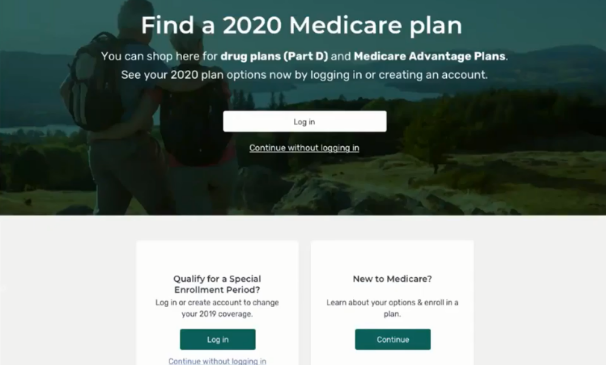
Star Ratings are displayed on the Medicare Plan Finder – which recently got a huge facelift – so seniors may consider both quality and cost in their enrollment decisions. In other words, Star Ratings are very important.
Other Key Findings
CMS also found that:
– More than 80 percent of beneficiaries are now enrolled in plans with 4 or more stars, up from 75 percent last year.
– This year, 141 plans earned higher 2020 ratings than they did in 2019.
– Only 57 health plans saw their overall ratings drop year-over-year.
– This year, 56 plans earned a4th star.
– Only 21 plans lost their 4th star this year.
– Approximately 52 percent of contracts for Medicare Advantage plans offering Part D coverage earned 4 stars or higher, compared to about 45% in 2019.
– Of 401 total plans for 2020, 210 are at 4 stars or higher, compared to 172 in 2019 when there were fewer plans – 376 to be exact.
– The comparison between 2020 and 2019 shows 55 contracts rated 3 stars for 2020 as opposed to 66 in 2019.
– The average star rating for a stand-alone prescription drug plan has improved from 3.34 in 2019 to 3.50 in 2020.
– There’s about 1,200 more Medicare Advantage plans operating in 2020 than in 2018, according to the Centers for Medicare and Medicaid Services.
What Can Your Health Plan Do Next Year?
If you didn’t achieve four stars this year, you have time to improve and influence your 2021 ratings with the right strategy, data, and attention to detail. It’s important that you review your current performance figures and use the right resources moving forward.
If you earned four stars this year – congratulations! However, now is not the time to sit back and relax. Star Ratings is a competitive process, and the health plans who get top billing have already started taking steps to ensure the same if not better performance next year.
Get Started
Tier 1 Pharmacy Consulting can work with your staff so everyone understands his or her responsibilities and how to successfully tackle them. We can help you develop a Star Ratings plan for 2021 that will help your health plan improve its performance and achieve your goals.
Tier 1 also will help you sort out conflicting messaging, outdated information, missing information, records and measures evaluated by CMS for its Star Ratings program. With us, you can rest assured that making changes doesn’t have to be complicated or overwhelming. It’s important that you earn the highest rating possible.
A four or five star rating is within your reach for 2021. We can help you get there.
About Tier 1
Tier 1 Pharmacy Consulting is a Denver, Colorado-based pharmacy benefit consulting firm offering customized services to healthcare plans that offer prescription drug benefits. Whether your health plan is big or small, Tier 1 offers strategic, cost-saving solutions that boost the plan’s overall value and help its members by providing high quality care.
Tier 1’s founder is a clinical pharmacist with more than a decade of experience in pharmacy benefit management. We are passionate about collaborating and developing effective strategies to improve health plan outcomes.
Tier 1 offers health plans a new perspective on how to manage their pharmacy benefit. Our team is made up of experts who strive to make effective plans even stronger and fill in any gaps due to a lack of time or resources.
We’re here for you. Drop us a note at info@tieronepc.com and let’s get connected.