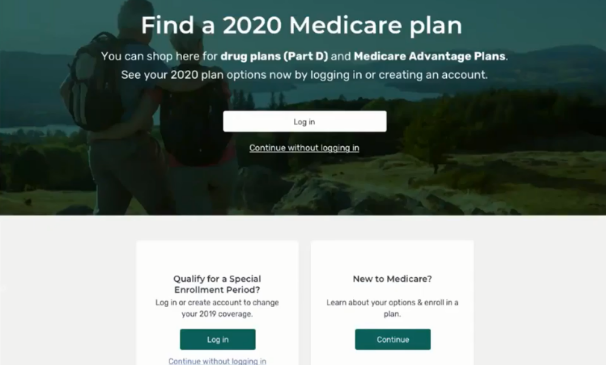
Seniors will have an easier time shopping for health plans and drug coverage thanks to a major overhaul of one of the government’s key online services.
The Centers for Medicare & Medicaid Services last month unveiled a new-and-improved Medicare Plan Finder on the Medicare.gov website. The move is part of the government agency’s eMedicare initiative to create a modern, personalized, and seamless customer experience for Medicare recipients.
It’s the first time in a decade that CMS has made changes to the system, and the new plan finder and related technology facelift comes just ahead of annual open enrollment when seniors begin in October to choose their plans for 2020.
A Needed Makeover
The plan finder upgrades include:
– A more simple login process to Medicare recipients’ online accounts.
– A fast drug list builder that reviews recipients’ prescriptions over the previous 12 months and suggests generic alternatives to name-brand drugs.
– More details on the different Medicare Advantage plans so seniors can easily compare benefits and choose the plan that is right for them.
– A guide for seniors to compare original Medicare, supplemental policies and Medicare Advantage plans, as well as up to three drug plans or three Medicare Advantage plans side-by-side.
Why Now?
In July, the Government Accountability Office (GAO) in a study determined that the Medicare Plan Finder was challenging for beneficiaries to navigate. It also provided incomplete information and information that was tough to find and even tougher to understand.
The Medicare Plan Finder was created to provide all of the health plans available in a person’s zip code, with crucial information about premiums and out-of-pocket costs, particularly for prescription drugs. Pricing is different for every health plan, so the tool aims to help consumers make informed decisions about what kind of health and pharmacy care plan they need – and how much they can afford. Plan Finder drug prices are updated regularly from October through August. Pricing for the current year is frozen in September in preparation for the new plan year’s display.
Under the changes, the new Plan Finder makes choosing a plan much easier and more user friendly. It’s also a welcome change for health plans, who have spent time and money trying to improve their own networks to offer people over age 65 private Medicare Advantage coverage, according to Forbes. Experts predict enrollment in private Advantage plans could rise as high as 70 percent between 2030 and 2040. If all goes as expected, the now easy-to-use Plan Finder could boost Medicare Advantage enrollment even further.
“The new Plan Finder walks users through the Medicare Advantage and Part D enrollment process from start to finish and allows people to view and compare many of the supplemental benefits that Medicare Advantage plans offer,” CMS said in a statement.
What Health Plans Need to Do
To keep the Plan Finder information current, Medicare requires health plans to submit files that update the costs of prescription drugs every two weeks. Many plans delegate this function to their PBM, but it’s important that health plans stay engaged in this process and ensure that there are effective processes to oversight these frequent submissions. Medicare wants to make sure enrollees are provided the most accurate information when making the decision on what prescription drug plan works best for them.
If a health plan fails to update its prescription drug pricing and other information, it could be suspended or removed from the Medicare Plan Finder. The plan won’t show up when consumers do a search using the tool, so they won’t even know your health plan exists. That means less money going into your health plan and an overall loss of revenue over time.
How We Can Help
The team at Tier 1 Pharmacy Consulting can be the liaison between the health plan and the pharmacy benefit manager to help oversee the steps needed to ensure CMS compliance, including regular updates to the Medicare Plan Finder. We can offer solutions on how to properly and effectively institute the appropriate process for oversight and ensure drug prices are, at all times, accurate and up-to-date all year. We are experts in Medicare. Avoid a Plan Finder suppression by partnering with us. We can help you stay compliant at all times, so you can focus on running your health plan.
About Tier 1
Tier 1 Pharmacy Consulting is a Denver, Colorado-based pharmacy benefit consulting firm offering customized services to healthcare plans that offer prescription drug benefits. Whether your health plan is big or small, Tier 1 offers strategic, cost-saving solutions that boost the plan’s overall value and help its members by providing high quality care.
Tier 1’s founder is a clinical pharmacist with more than a decade of experience in pharmacy benefit management. We are passionate about collaborating and developing effective strategies to improve health plan outcomes.
Tier 1 offers health plans a new perspective on how to manage their pharmacy benefit. Our team is made up of experts who strive to make effective plans even stronger and fill in any gaps due to a lack of time or resources.
We’re here for you. Drop us a note at info@tieronepc.com and let’s get connected.