Last month, HPMS released a memo outlining its 2020 Readiness Checklist for Medicare Advantage Organizations and prescription drug plans.
The Centers for Medicare and Medicaid Services recommends all Medicare Advantage and prescription drug plans review the checklist – and take the appropriate action to meet the requirements next year. Health plans should closely review the entire checklist to ensure compliance. Remember, the checklist isn’t a compilation of suggestions from the government. Instead, it’s a summary of the most critical requirements.
Here’s a few examples of what’s in the readiness checklist for 2020:
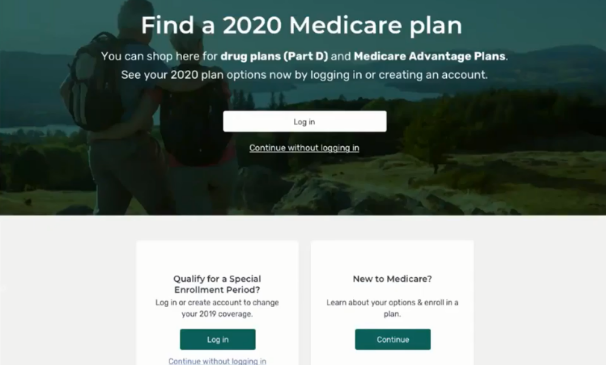
Medicare Plan Finder Data. Part D Sponsors must provide access to the Health Plan Management System Part D Pricing File Submission Module.
Prescription Drug Event Requirements. Part D Sponsors must submit the data CMS needs to carry out payment provisions through the Prescription Drug Front-End System and processed by the Drug Data Processing System.
Coverage Gap Discount Program. The agency is asking Part D Sponsors to understand their responsibilities to participate in the CGDP, and provides information about the CGDP portal, onboarding training and more.
Precluded Providers and Prescribers. CMS has bigger expectations for 2020 when it comes to managing precluded providers and prescribers. Moving forward, MAOs/Part D Sponsors must, when when a prescriber is on the Preclusion List, deny payments for reject a pharmacy claim, deny a beneficiary request for reimbursement, or deny a health care service.
What Can Your Health Plan Do Next Year?
Tier 1 Pharmacy Consuting can make a readiness assessment for your health plan or prescription drug plan to ensure you are prepared and identify potential problems before they begin.
Get Started
Tier 1 Pharmacy Consulting can work with your staff so everyone understands his or her responsibilities and how to successfully tackle them. We can help you develop a Star Ratings plan for 2021 that will help your health plan improve its performance and achieve your goals.
Tier 1 also will help you sort out conflicting messaging, outdated information, missing information, records and measures evaluated by CMS for its Star Ratings program. With us, you can rest assured that making changes doesn’t have to be complicated or overwhelming. It’s important that you earn the highest rating possible.
A four or five star rating is within your reach for 2021. We can help you get there.
About Tier 1
Tier 1 Pharmacy Consulting is a Denver, Colorado-based pharmacy benefit consulting firm offering customized services to healthcare plans that offer prescription drug benefits. Whether your health plan is big or small, Tier 1 offers strategic, cost-saving solutions that boost the plan’s overall value and help its members by providing high quality care.
Tier 1’s founder is a clinical pharmacist with more than a decade of experience in pharmacy benefit management. We are passionate about collaborating and developing effective strategies to improve health plan outcomes.
Tier 1 offers health plans a new perspective on how to manage their pharmacy benefit. Our team is made up of experts who strive to make effective plans even stronger and fill in any gaps due to a lack of time or resources.
We’re here for you. Drop us a note at info@tieronepc.com and let’s get connected.